Bimonthly assessment for the month of February
Bimonthly assessment for the month of feb 2021
Problem representation and anatomical localization :
➡️Running into the objects ,drooping of eyelids --EYELID OPENING APRAXIA —
Possible causes and anatomical localization include -
Muscles involved in opening eyelids
➡️levator palpebrae superioris-LPS is supplied by occulomotor nerve
➡️Mullers muscle
➡️Frontalis muscle
cerebral cortex, basal ganglia, and superior colliculus (SC) are thought to play a role in disinhibition of leavator palpebra superioris
➡️Orbicularis oculi -closes eyelids
➡️Cerebral cortex -provides promotor control for eyelid movements,medial frontal lobes including supplementary area involved in control of blinking
➡️Substabtia Nigra pars reticulata-dopamine depletion decreases blink rate -SEEN WITH PARKINSON PATIENT .
➡️superior colliculus
EYELID DISORDERS - Droopy eyelids can be caused by neurogenic -innervational failure or LPS damage -myogenic Ptosis
Causes of neurogenic ptosis include :
third cranial nerve palsy
➡️Horner syndrome
➡️Myasthenia gravies
➡️botulism
➡️ Gullian Barre syndrome
➡️chronic inflammatory demyelinating polyneuropathy
MYOGENIC PTOSIS :
➡️Congenital ptosis
➡️Eyelid trauma /surgery
➡️Mitochondrial myopathy
➡️Oculi pharyngeal dystrophy
➡️Myotonic dystrophy
➡️Herpes zoster
➡️Chronic topical steroid use
History of frequent falls :
Falls in elderly patient with background history of slowness and decreased expressiveness - would suggest autonomic instability or postural instability seen with parkinson patient .
Cause of falls :
➡️Ataxial rigidity
➡️Bradykinesia
➡️ Loss of postural reflexes
➡️Freezing
➡️ Visual vestibular component
B) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
Treatment :
1 . Tab. SYNDOPA 110mg PO TID
2. Tab. METFORMIN 500mg PO OD
Metformin MOA -
➡️Decreases hepatic gluconeogenesis
➡️Increases peripheral uptake of glucose
➡️Increases insulin sensitivity
2) Patient was apparently asymptomatic 2 years back then he developed weakness in the right upper and lower limb, loss of speech.
More here: https://ashfaqtaj098.blogspot.com/2021/02/60-year-old-male-patient-with-hrref.html?m=1
a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
A) systolic heart failure
B)diastolic heart failure
His examination findings were Visible apical impulse, Pericardial bulge, visible pulsations, dilated veinsshift of apex beat to 6th ICS, Thrill at the apex, Loud S1 present, loud P2 present, S3 Accentuating on inspiration- RVS3, Expiration - LVS3
His Ecg shows poor R wave progression
Chest Xray PA shows Cardiomegaly
His 2Echo is suggestive of Heart failure DCMP with Hypokinesia at RCA, LCX
Anatomical diagnosis:
The location to his problems is at the Heart, secondary to atherosclerosis of the vessels
Risk factors:
Alcohol
Age of 60 years
Male gender
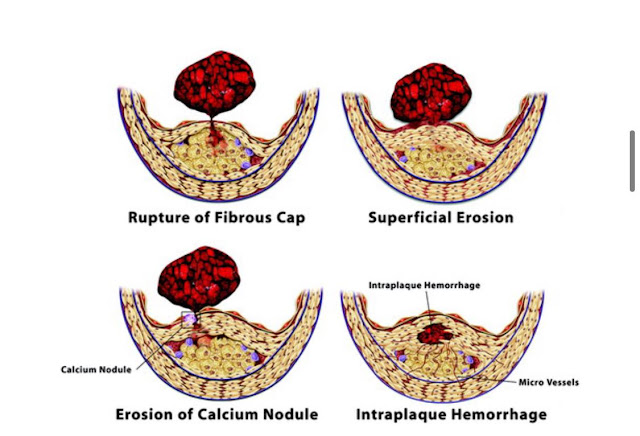
'In vivo imaging techniques applied in humans and the success of antithrombotic and fibrinolytic therapy in ACS established in practice the role of thrombosis in their pathogenesis. A number of microanatomic mechanisms underlie acute coronary thrombosis. According to autopsy studies—clearly biased toward fatal outcomes—a through-and-through rupture of the plaque’s protective fibrous cap most commonly causes lethal coronary thrombosis. Other mechanisms that account for a minority of fatal coronary thromboses include superficial erosion, intraplaque hemorrhage, and the erosion of a calcified nodule. Thus, physical disruption of the atherosclerotic plaque accounts for almost all acute coronary thromboses.'
'Disrupted plaques provoke thrombosis in several ways. First, contact with collagen in the plaque’s extracellular matrix can trigger platelet activation. Second, TF produced by macrophages and SMCs activates the coagulation cascade. The disrupted plaque thereby represents a “solid-state” stimulus to both thrombosis and coagulation; these pathways reinforce each other, as thrombin generation amplifies the activation of platelets and other cells in the lesion. Conversion of fibrinogen to fibrin and release of von Willebrand factor from activated platelets can provide the cross-linking molecular bridges between platelets that yield the dense, 3-dimensional network of platelets entrapped in fibrin characteristic of the “white” arterial thrombus.'
What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
Etiologies - 1.coronary heart disease -ICMP
2.Cardiomyopathies -DCMP
3. Valvular heart disease - predominantly left side
With no revelant history of smoking and also no wheeze,no seasonal variations -respiratory cause of sob has been ruled out .
Sequence of events :
2 years back weakness of right upper and lower limb with brocas aphasia
F/b
2 months history of SO,pedal edema
- What is the efficacy of each of the drugs listed in his current treatment plan
1.Tab. Lasix 40 mg bd
2.Tab. Benfomet plus od
3.Tab. Telma 40 mg od
4.Tab. Met xl 50mg od
5.Tab. Aldactone 25mg od
6.Salt restriction <2gm/day
7.Fluid restriction<1.5lit/day
Lasix ,fluid and salt restriction are supportive management to decrease preload on the heart .
Spirinolactone + Telmisartan + beta blockers are now recommended therapy for the patient’s with -chronic heart failure with reduced ejection fraction according to recent guidelines .
Most efficacious is ARNI + other combination .
We will screen for CAD - as patient falls under high risk for CAD
General -pallor +
Systemic examination - no obvious findings of pneumonia
ECG and echo showed no evidence of CAD ,
Concentric LVH with EF -62 percent .
X ray - bilateral pleural effusion with no consolidators changes .
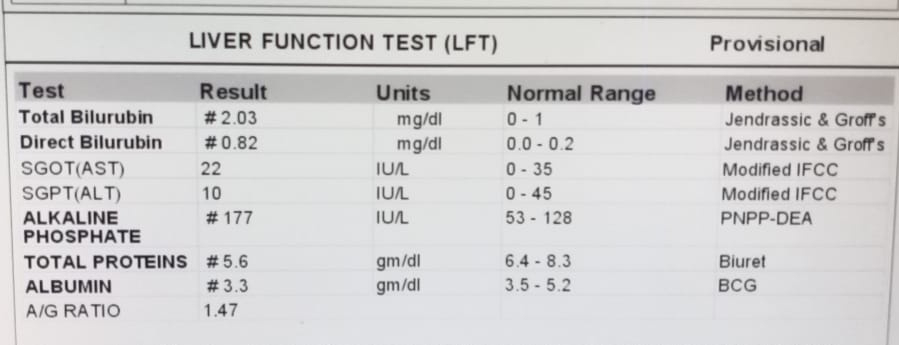
Hemogram showed dimorphism anemia ( mostly due to Iron and vitB12 deficiency - Nutritional deficiency )
Etiology - Dimorphic anemia secondary to iron and vit B12 deficiency
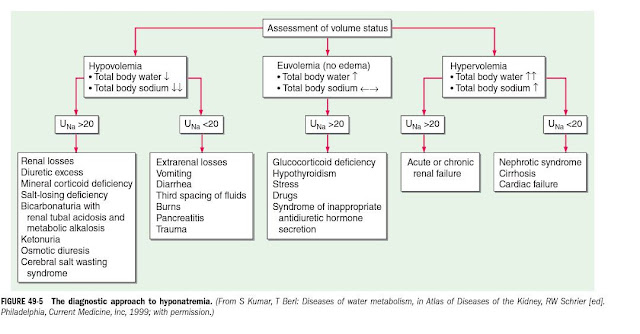
Patient after admission suddenly developed hyponatremia .
Approach to hyponatremia
c) What is the efficacy of each of the drugs listed in his current treatment plan especially for his hyponatremia? What is the efficacy of Vaptans over placebo? Can one give both 3% sodium as well as vaptan the same pt?