a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?How specific is his dilated superficial Abdominal vein in making diagnosis?
About his superficial abdominal veins :
For a long term alcoholic, he could be a risk factor to develop portal hypertension, which may be present with superficial abdominal veins and varices
➡️Triad of portal hypertension :
Bacterial peritonitis
Hepatic enceohalopathy
Cirrhotic Hepatopulmonary syndrome
Portopulmonary hypertension
Other differentials include:
➡️Caput medusae due to portal hypertension
➡️Dilated veins in IVC
➡️Congenital
➡️Obstruction of IVC
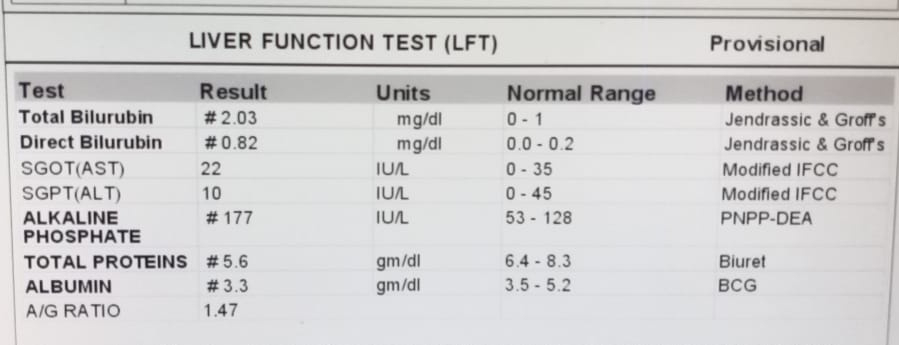
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? What is the cause of his hypoalbuminemia?Why is the SAAG low?
c)Will PT,INR derangement preceed hypoalbuminemia in liver dysfunction??Share reference articles if any!
The liver plays a central role in the clotting process, and acute and chronic liver diseases are invariably associated with coagulation disorders due to multiple causes: decreased synthesis of clotting and inhibitor factors, decreased clearance of activated factors, quantitative and qualitative platelet defects, hyperfibrinolysis, and accelerated intravascular coagulation.
https://www.medscape.com/answers/177354-36077/what-is-the-role-of-prothrombin-time-pt-in-the-evaluation-of-acute-liver-failure
Yes,Inflammation and infection .
Albumin is considered a negative acute phase reactant, which means that as inflammation and other acute physiologic processes occur, its levels decrease
In liver disease:Albumin is synthesized in the liver, and low serum albumin can be indicative of liver failure or diseases such as cirrhosis and chronic hepatitis. If present, hypoalbuminemia is generally considered to be a sign of advanced hepatic cirrhosis, or irreversible damage to the liver
Malnutrition or malabsorption
Low albumin levels can also indicate chronic malnutrition from protein losing enteropathy.
This is often caused or exacerbated by ulcerative colitis,but can also be seen in cardiac disease and systemic lupus erythematosus
f) What is the efficacy of each of the drugs listed in his current treatment plan
QUESTION 2
A 45 year old female with complaints of abdominal distension since 2 years and pedal edema since 2 months, with increasing distension causing difficulty in eating drinking ,though she has a good appetite and able to fulfill it.
a). What is the problem representation of this patient and what is the anatomical localization for her current problem based on the clinical findings?
She is a k/c/o DM since 1 year.she took medication for 6 months and later she stopped taking the medication.
All of the above complaints point to liver pathology.
b) What is the etiology of her refractory ascites and pleural effusion? and how would you as a member of the treating team arrive at a diagnosis?
Refractory ascites is defined as:
Ascites that does not recede or that recurs shortly after therapeutic paracentesis, despite sodium restriction and diuretic treatment. To date, there is no approved medical therapy specifically for refractory ascitis
The diagnostic criteria of refractory ascites consist of:
Ascites that cannot be mobilized with early recurrence within 4 weeks of abdominal paracentesis and lack of response to maximal doses of diuretic (spironolactone 400 mg/d and furosemide 160 mg/d) for at least 1 week.
c) Approach to a patient with ascites?
The etiology of the ascites is best determined by paracentesis, a bedside procedure in which a needle or small catheter is passed transcutaneously to extract ascitic fluid from the peritoneum. The ascitic fluid should be sent for measurement of albumin and total protein levels, white cell count with differentials, and, if an infection is suspected, Gram's stain and culture, with inoculation into blood culture bottles at the patient's bedside to maximize the yield. A serum albumin level should be measured simultaneously to permit the calculation of the serum-ascites albumin gradient (SAAG) [9].
Cytology can be useful in the diagnosis of peritoneal carcinomatosis. Tuberculous peritonitis is typically associated with ascitic fluid lymphocytosis but can be difficult to diagnose by paracentesis. A smear for acid-fast bacilli (AFB) has a diagnostic sensitivity of only 0 to 3%; a culture increases the sensitivity to 35–50%. In patients without cirrhosis, an elevated ascitic adenosine deaminase level has a sensitivity (SN) of >90% when a cut-off value of 30–45 U/L is used. When the cause of ascites remains uncertain, laparotomy or laparoscopy with peritoneal biopsies for histology and culture remains the gold standard [9].
Clinically is there any way to differentiate pre hepatic, post hepatic and hepatic causes?
d)Causes of budd chiari syndrome?
Why did the patient undergo bone biopsy?
Why did the patient undergo bone biopsy?
d) Management strategies for refractory ascites and Budd chiari syndrome? Share the potential advantages and disadvantages of Peritoneal dialysis catheter placement in refractory ascites?
e) What is the efficacy of each of the drugs listed in his current treatment plan
f)What is the current outcome?and what could be the etiology of her current outcome?
QUESTION 3
55year old male with SOB and abdominal distension,orthopnea
a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Ans:
Problem representation:
Abdominal distention with scrotal swelling since 1 week
SOB grade IV since 4 days
SOB on lying down since 3days
Pedal edema since 3 days
Anatomical Localization:
Features like Pedal edema, Ascites, Orthopnea suggest Heart (Right heart failure)
His current problem:
Cor Pulmonale with severe PAH Grade III with AKI, Congestive hepatomegaly & gross ascites.
Above symptoms have aggravated since 1 week associated with constipation since 1 week, relieved on taking medication.
Decreased urine output intermittently, facial puffiness and anasarca relieved on medication.
Symptoms increased on intake of alcohol, non adherence to diet.
b) What is the etiology of his ascites? and how would you as a member of the treating team arrive at a diagnosis?Chart out the sequence of events!
c)What is the efficacy of each of the drugs listed in his treatment plan?
d)What are his current outcomes ?
QUESTION 4
4)Please go through the thesis presentation below and answer the questions below by also discussing them with the presenter
a)What was the research question in the above thesis presentation?
SAAG and ITS UTILITY
)What is the current available sensitivity and specificity of SAAG in diagnosis of etiology of ascites
5) Journal club questions on Ascites theme
STUDY DESIGN
Institution-based cross-sectional study.
THESIS IS ABOUT:
CLINICAL PROFILE,EVALUATION,DIAGNOSIS AND THERAPEUTIC OUTCOMES IN PATIENTS WITH ASCITES
STUDY DESIGN
Prospective study, Qualitative, Non Experimental